Another stick, Another article, Another arrow pointing me ahead
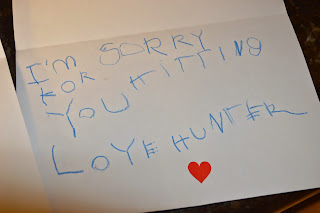
Hunter had a great couple of weeks post-steroid, as I blogged about previously, and then we saw a gradual decline. There are, however, multiple times a day that I say "WOW!" in my head, because I am amazed at the perfect question or comment that comes out of his mouth. I called our amazing pediatrician and asked if I could bring him in for labs, since he seemed to be having a flare. I wanted to compare the labs we ran in June and see if any of the numbers increased or continued to decrease.
Here's lab #1, complete with Anti-DNase B Strep Antibodies, the CBC, and the Coxsackie IgG (Hand/foot/mouth disease). These all had been elevated the first time labs were run by the DAN/Immunologist dr. The second time, in June, some of them had decreased. Here is the most recent lab:

The Strep number was <76 the last time we ran labs in June, and the Coxsackie number was elevated as well. Dr V explained to me that there are several strains of Coxsackie. She thought the numbers just implied that he had the virus in the past. In order to measure the amount, they dilute the serum until it shows a negative response. For Hunter, for a few of the tests, they had to dilute it up to 1600 times before it was negative (should have taken less than 100 times). The IgG is the antibody that indicates if the patient has had the virus in the past. The IGM raises quickly if it is an acute infection.
So the only other item elevated was Monocytes. I had no idea what a monocyte was, or what significance it had if elevated. Google is an amazing tool- sometimes my best friend, sometimes my worst enemy...
(from Diagnoseme.com)
An increased number of monocytes in the blood (monocytosis) occurs in response to chronic infections, in autoimmune disorders, in blood disorders, and in cancers.
Diagnosis and Tests
An increased percentage of monocytes may indicate:
I can't believe I just found another immune system component! Snap that piece into the puzzle.
Here is the second form from his labs:
So his HHV (Human Herpes Virus) was elevated again. In June, it showed that his HHV igg went from 8.46 to 1.43. This time, it is at 5.37. Normal range is >.99.
Why are these labs elevated again? He shows no signs of a virus, no signs of an illness...yet he maintains numbers that fluctuate in and out of the normal range.
So here is the kicker. The blow it out of the park, home-run type of article. My good friend Jenny sent it to me and I stood in the kitchen, jaw dropped open, as I read it. By Monday I will have found contact information for not only the author, but for all of the major researchers involved in this project.
http://www.nytimes.com/2012/08/26/opinion/sunday/immune-disorders-and-autism.html?_r=3&pagewanted=all
In a nutshell, this article attempts to prove my original hypothesis- that there was an autoimmune component attached to Hunter's PDD-NOS diagnosis. Here are a few of the main points(straight from the article- not my words):
Here's lab #1, complete with Anti-DNase B Strep Antibodies, the CBC, and the Coxsackie IgG (Hand/foot/mouth disease). These all had been elevated the first time labs were run by the DAN/Immunologist dr. The second time, in June, some of them had decreased. Here is the most recent lab:

The Strep number was <76 the last time we ran labs in June, and the Coxsackie number was elevated as well. Dr V explained to me that there are several strains of Coxsackie. She thought the numbers just implied that he had the virus in the past. In order to measure the amount, they dilute the serum until it shows a negative response. For Hunter, for a few of the tests, they had to dilute it up to 1600 times before it was negative (should have taken less than 100 times). The IgG is the antibody that indicates if the patient has had the virus in the past. The IGM raises quickly if it is an acute infection.
So the only other item elevated was Monocytes. I had no idea what a monocyte was, or what significance it had if elevated. Google is an amazing tool- sometimes my best friend, sometimes my worst enemy...
(from Diagnoseme.com)
Causes and Development
Diagnosis and Tests
An increased percentage of monocytes may indicate:
- Chronic inflammatory disease
- Parasitic infection
- Tuberculosis
- Viral infection (for example, infectious mononucleosis, mumps, measles)
I can't believe I just found another immune system component! Snap that piece into the puzzle.
Here is the second form from his labs:
So his HHV (Human Herpes Virus) was elevated again. In June, it showed that his HHV igg went from 8.46 to 1.43. This time, it is at 5.37. Normal range is >.99.
Why are these labs elevated again? He shows no signs of a virus, no signs of an illness...yet he maintains numbers that fluctuate in and out of the normal range.
So here is the kicker. The blow it out of the park, home-run type of article. My good friend Jenny sent it to me and I stood in the kitchen, jaw dropped open, as I read it. By Monday I will have found contact information for not only the author, but for all of the major researchers involved in this project.
http://www.nytimes.com/2012/08/26/opinion/sunday/immune-disorders-and-autism.html?_r=3&pagewanted=all
In a nutshell, this article attempts to prove my original hypothesis- that there was an autoimmune component attached to Hunter's PDD-NOS diagnosis. Here are a few of the main points(straight from the article- not my words):
"So here’s the short of it: At least a subset of autism — perhaps one-third, and very likely more — looks like a type of inflammatory disease. And it begins in the womb.
It starts with what scientists call immune dysregulation. Ideally, your immune system should operate like an enlightened action hero, meting out inflammation precisely, accurately and with deadly force when necessary, but then quickly returning to a Zen-like calm. Doing so requires an optimal balance of pro- and anti-inflammatory muscle.
In autistic individuals, the immune system fails at this balancing act. Inflammatory signals dominate. Anti-inflammatory ones are inadequate. A state of chronic activation prevails. And the more skewed toward inflammation, the more acute the autistic symptoms."
"Better clues to the causes of the autism phenomenon come from parallel “epidemics.” The prevalence of inflammatory diseases in general has increased significantly in the past 60 years. As a group, they include asthma, now estimated to affect 1 in 10 children — at least double the prevalence of 1980 — and autoimmune disorders, which afflict 1 in 20.
Both are linked to autism, especially in the mother. One large Danish study, which included nearly 700,000 births over a decade, found that a mother’s rheumatoid arthritis, a degenerative disease of the joints, elevated a child’s risk of autism by 80 percent. Her celiac disease, an inflammatory disease prompted by proteins in wheat and other grains, increased it 350 percent. Genetic studies tell a similar tale. Gene variants associated with autoimmune disease — genes of the immune system — also increase the risk of autism, especially when they occur in the mother. "
**I could not tolerate wheat during any pregnancies. I actually developed some food allergies during Paige's pregnancy. My father has Celiac and Hunter is Category 8 Risk for developing Celiac (the highest possible number).
"Debate swirls around the reality of the autism phenomenon, and rightly so. Diagnostic criteria have changed repeatedly, and awareness has increased. How much — if any — of the “autism epidemic” is real, how much artifact? YET when you consider that, as a whole, diseases of immune dysregulation have increased in the past 60 years — and that these disorders are linked to autism — the question seems a little moot. The better question is: Why are we so prone to inflammatory disorders? What has happened to the modern immune system? There’s a good evolutionary answer to that query, it turns out. Scientists have repeatedly observed that people living in environments that resemble our evolutionary past, full of microbes and parasites, don’t suffer from inflammatory diseases as frequently as we do. Generally speaking, autism also follows this pattern. It seems to be less prevalent in the developing world. Usually, epidemiologists fault lack of diagnosis for the apparent absence. A dearth of expertise in the disorder, the argument goes, gives a false impression of scarcity. Yet at least one Western doctor who specializes in autism has explicitly noted that, in a Cambodian population rife with parasites and acute infections, autism was nearly nonexistent.
For autoimmune and allergic diseases linked to autism, meanwhile, the evidence is compelling. In environments that resemble the world of yore, the immune system is much less prone to diseases of dysregulation. "
The author goes on to describe the mother's immune system dysregulation, and the effect it can have on a child's brain development. The guilt factor has re-entered my mind. We went from Paige, who was born 8 weeks early, spent 31 days in the NICU, and basically scared us to ever go anywhere without our bottle of hand sanitizer. I used to clean her toys on a 3 day cycle, have check-lists of what to sterilize on which day, and didn't let a germ invade our house for her entire first year of life. I became pregnant with Hunter when she was 10 months old. What if I was "too clean" for his development?
If we created a child who had a weakened immune system, partly due to genetics, and then had an autoimmune response when the germs attacked his body at 17 months, would Autism be the result? Would eczema be an autoimmune response? Would vitiligo and Celiac be these continued responses?
Time to stalk Moises Velasquez-Manoff, the author of “An Epidemic of Absence: A New Way of Understanding Allergies and Autoimmune Diseases” on google.


Comments
Post a Comment