Finding the Magician
I need to back up a few weeks to June- haven't blogged about it yet for several reasons, but am ready to throw it all out there.
I rarely read the Parents Magazines that I get in the mail- it's not that I don't find them valuable or informative, I just can't find the time. For some reason, I picked up an issue from May I believe, and saw PANDAS on the front cover. I couldn't believe it- I frantically searched through the magazine to find the article. The link is below:
http://www.parents.com/kids/health/other-health-issues/pandas-syndrome/
In the article, a family described their experience and mentioned that their specialist, a pediatrician from Chicago, basically saved their lives.
Hmm....Chicago...heading up North in July...could there possibly be an opening to see him?
I called and found out that Dr. K was out of the country. He would be returning the day before Peter and I returned on our trip from Turks and Caicos. He was booked solid.
So I resorted to begging and pleading. OK, not really, but I am sure she heard my voice waver and could imagine the tears in my eyes. She called me back an hour later and worked us in at lunchtime. She knew we would be headed back home on Tuesday, so Monday was our only shot.
Dr. K is an expert in PANDAS. He lives, breathes, and studies it. He travels all over the world to meet with families, present, and study the very hypothesis that I have been contemplating.
He lists on his website several characteristics of classic PANDAS- Hunter doesn't meet all the criteria, but several of the key ones are listed below. I've highlighted the symptoms that Hunter displays. Please read past all of the boxed text- I couldn't figure out how to delete it but I have continued the blog under it...
I rarely read the Parents Magazines that I get in the mail- it's not that I don't find them valuable or informative, I just can't find the time. For some reason, I picked up an issue from May I believe, and saw PANDAS on the front cover. I couldn't believe it- I frantically searched through the magazine to find the article. The link is below:
http://www.parents.com/kids/health/other-health-issues/pandas-syndrome/
In the article, a family described their experience and mentioned that their specialist, a pediatrician from Chicago, basically saved their lives.
Hmm....Chicago...heading up North in July...could there possibly be an opening to see him?
I called and found out that Dr. K was out of the country. He would be returning the day before Peter and I returned on our trip from Turks and Caicos. He was booked solid.
So I resorted to begging and pleading. OK, not really, but I am sure she heard my voice waver and could imagine the tears in my eyes. She called me back an hour later and worked us in at lunchtime. She knew we would be headed back home on Tuesday, so Monday was our only shot.
Dr. K is an expert in PANDAS. He lives, breathes, and studies it. He travels all over the world to meet with families, present, and study the very hypothesis that I have been contemplating.
He lists on his website several characteristics of classic PANDAS- Hunter doesn't meet all the criteria, but several of the key ones are listed below. I've highlighted the symptoms that Hunter displays. Please read past all of the boxed text- I couldn't figure out how to delete it but I have continued the blog under it...
| Controversial and still highly contentious concepts of PANDAS (Paediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococci) and PITAND (Paediatric Infection-triggered Autoimmune Neuropsychiatric Disorders) were introduced by A. J. Allen and Swedo et al. in the late nineties. The premise brought forward by these researchers, that certain mental illnesses (e.g. Obsessive-compulsive disorder, tic disorders including certain cases of Tourette's syndrome) can be caused by an infection with a common infectious agent (designated as "PANDAS": Group A beta-hemolytic Streptococcus - GABHS) and (possibly) by other infectious agents (designated as "PITAND": certain viruses, Mycoplasma pneumonie, etc.), severely challenges a century of Freudian "devotion" of the medical community. In a simple language, theories of Allen and Swedo are bringing the mental illness back to its biological roots and essentially define it as a physical illness with mental symptoms. Recent scientific evidences are widening the list of possible mental illnesses that could be included into PANDAS and PITAND group. Certain cases of Anorexia nervosa (see the footnote below), psychotic symptoms following the Lyme disease and at least some cases of Autistic Spectrum Disorders (PDD NOS) have all been linked to an infectious agent and their pathophysiology appears compatible with PANDAS and PITAND syndromes. | ||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||
| Suggested diagnostic criteria for PANDAS: | ||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||
| Separation anxiety Type 1 (person-dependent): patient's dependence on parents (most likely mother) that appears clearly inappropriate for patient's chronological age. | ||||||||||||||||||||||||||||
| ** Separation anxiety Type 2 (environment-dependent): patient severely dependent on certain (familiar) environment(s) (i.e., home). When offered any social interaction outside home pr | ||||||||||||||||||||||||||||
| We are currently working out an acceptable diagnostic formula for PANDAS patients. Please consider this "work in progress" ! | ||||||||||||||||||||||||||||
| ||||||||||||||||||||||||||||
| So, What is This All About? | ||||||||||||||||||||||||||||
| The most exciting prospect of PANDAS and PITAND theory is realization that a biological agent(s) (in this case, an infectious vector) has been identified as a single cause of a mental illness. PANDAS and (possibly) PITAND do indeed represent a disease(s) that satisfies the McGovern and Troisi criteria (please refer to Autism page). Various descriptive terms so much abused in current scientific terminology of mental illnesses ("chemical imbalance", "abnormal brain chemistry", etc.) that have absolutely no scientific meaning nor diagnostic or therapeutic value, might be finally relegated to history. It is likely that following a century of unsuccessful search for the disease of the mind, the body will be where the answers shall be found. | ||||||||||||||||||||||||||||
| Once the cause of an illness (in this case a mental illness) has been identified, search for an adequate treatment is the next logical step. In PANDAS and PITAND syndromes an adequate treatment already exists and has been proven successful. Use of antibiotics for GABHS infection (i.e. Penicillin) does not only "control" the symptoms but, in certain cases, may cure the patient. Once however, the damage to the nervous system has been demonstrated (both in PANDAS and PITAND) further treatments modalities may be necessary, and these are readily available as well (corticosteroids, Intravenous immunoglobulin, anti-inflammatory compounds other than steroids, etc.). It is also extremely important to mention that the resulting damage to the nervous system symptomatic of PANDAS and PITAND syndromes can be reversed in its early stages (please refer to our Bibliography page), and a complete cure can be expected. It is likely that with the passage of time and an increased acceptance of Allen's and Swedo's theories, a definite cause of a number of mental illnesses overwhelming the modern society will be defined and (possibly) true cures achieved. | ||||||||||||||||||||||||||||
| Review of currently available treatments for PANDAS | ||||||||||||||||||||||||||||
| Antibiotics | ||||||||||||||||||||||||||||
| Antibiotics have been the mainstay of PANDAS treatment (together with SSRIs). The idea behind use of antibiotics is the eradication of Group A beta hemolytic Streptococcus. Unfortunately, the results have been mixed at best what corresponds to our professional experiences with PANDAS patients as well. We have seen severely symptomatic patients who have had negative antibody titers for Strept and at the same we have seen at least one patient whose symptoms have disappeared completely following the antibiotic treatment despite of persistence of high Strept antibody titers. It is entirely possible and even likely that use of antibiotics in the early stages of PANDAS could result in a complete recovery. ADDENDUM: We have followed several patients in whom the initial antibiotic treatment resulted in a complete symptoms resolution for almost 6 years. Unfortunately, ALL of these patients eventually had a recurrence and had to be treated with the IVIG. Thus, it is our experience that eventually ALL patients with PANDAS will eventually become antibiotic non-responders and other therapeutic option must be considered. Thus, long-term full-dose antibiotic treatment for PANDAS does not appear to be a viable option! ADDENDUM: Another possible explanation for the initial effectiveness of antibiotics in PANDAS may be the presumed neuroprotection as a result of an increased glutamate transporter expression (with use of beta-lactam antibiotics; Rothstein, J. D. et al, Letters to Nature, Nature Vol 433; 6 January 2005). | ||||||||||||||||||||||||||||
| Corticosteroids | ||||||||||||||||||||||||||||
| Just the fact that the "steroid burst" (used to test possible future effectiveness of IVIG) tend to control PANDAS symptoms effectively brings it into consideration as a possible treatment for PANDAS. Since the short-term steroid treatment only controls the symptoms temporarily (upon cessation of the treatment full return of symptoms is almost a rule!) and the prolonged use of it may have rather serious side effects, corticosteroids have not been (and should not be) used as a treatment in PANDAS. | ||||||||||||||||||||||||||||
| Removal of adenoids and tonsils | ||||||||||||||||||||||||||||
| At least one recent study reports symptom resolution in patients with PANDAS following a surgical removal of tonsils and/or adenoids. Since the fore said study had only limited time follow-up of these patients, the success (and the future failure) of this treatment is likely to parallel the results of antibiotic treatment(s). | ||||||||||||||||||||||||||||
| . | ||||||||||||||||||||||||||||
| IVIG | ||||||||||||||||||||||||||||
| In a carefully selected group of patients the effectiveness of the IVIG treatment in PANDAS patients appears excellent. It has been our experience that a complete and lasting recovery can and should be expected within days or weeks following the treatment (please check PANDAS clinical cases page) in 80%+ of patients. This, relatively safe procedure can be done in an outpatient setting thus avoiding additional trauma to the child and his/her parents. Unfortunately the serious drawback to this treatment is its cost and the fact that many insurance companies have not covered it until now. Recently however, several insurance carriers have started to cover the cost of the infusion. If you wish to learn more about this treatment please refer to our IVIG page! |
I had a hard time pasting the information from his site, so here is the link to the address is the information above doesn't make sense:
So... we flew home to Chicago Sunday, and turned back around the next morning to take Hunter to see Dr K, or "the wizard." I taped our conversation so I could transcribe it when we got home, but basically here are a few of the key points:
- Hunter immediately gave him eye contact, looked at him, not "through him". Said there "are several things that are suspicious. It should take us over to PANDAS diagnosis. He started with TICS. As a rule, AU never ever starts with Tics. I have never seen AU start with Tics.
-Sensitivity to clothing, labels, etc- yes, it is present in AU, but it is almost uniformally present in PANDAS.
-Elevated strep titers.
-Other autoimmune components- intolerance to gluten, eczema, vitiligo
-Typically the father of an AU child is older; the mother of a PANDAS child is me :)- a little OCD, high anxiety, etc.
-said PDD-NOS is a garbage term for "something is wrong with your child, but we don't really know what it is."
-Next step- steroid burst. Give steroids for 5 days and then keep observations for 2-3 weeks. See if the results are indicative of measurable clinical improvement.
I asked him about the diagnosis...
"I believe that chances that he has PPD-NOS not as a garbage term but as a part of AU is minimal. It is most likely that he has PANDAS. And it is going to be confirmed by this. Since he didn’t have an MRI done there is an outside possibility that the episode he did have would be viral encephalitis, or any of this, that could cause damage to the brain and indirectly cause the symptoms. Interestingly enough the approach between PANDAS and encephalitis, in pandas we believe that one treatment in PANDAS is sufficient, but if we have MRI done and see damage, you generally need at least three treatments to recover."
So what did we do?
After more research, consultation, and prayers, we started the steroids. If you have ever had your children on steroids, you know what fun we had for a week. Disturbed sleep, mood swings, aggression...auggh! I sent Dr. K an email and indicated that we had gone backwards. His reply? "WE MUST WAIT TWO WEEKS.'
Two weeks post and we realized we saw our son again. He answered questions appropriately. He looked at me without a prompt. He would have fits, but they would be typical four-year-old fits. His brain just seemed to "work." He didn't have any staring spells. He initiated play with peers that he had never initiated with before. And all of these observations were noted by myself and Peter, with the absence of ABA therapy and supplements. Our nanny, who didn't know about the steroid burst, commented after the second week that he had remarkable changes in his behavior, he attended to tasks for longer periods of time, and he seemed focused. She said the same thing Peter did- "his brain was working."
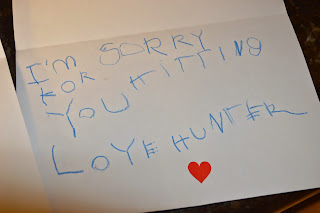
Today marks four weeks post steroid, and I have lost that loving feeling. He has hit me twice in the past two days. He had a staring spell at our neighbor's house a few days ago. His pupils are again dilated. He dumps toys and then moves on to the next. He has become obsessive over the ipad, the phone, and going to Target more so than before. During our diagnostic phase with the steroid, if we told him his time was up, there was not an all-out brawl. And the nanny told me one day he told her (after his two shows) that she could turn the TV off now. WHAT??? He would watch TV all day long if I would allow him to (which is why I am such a stickler on that tube being off!).
We found the magician, the one who brought me back to the little boy I knew prior to his illness. Steroids are short-lived, short-term, not permanent; however you want to say it. I know that I want him back for the long-term. I want to see those eyes alive again like I did in those two weeks. I don't know if IVIG is the answer or if any improvement would show after the recommended procedure, but I do know that this autoimmune component is real. I didn't imagine my son as normal prior to the virus. I didn't wake up the next day and imagine him with a tic. I didn't imagine him walking on his toes the next week. And I for surely did not imagine him with an Autism Spectrum Disorder.
Please pray for our minds, our hearts, and our decisions in the future.

Comments
Post a Comment